- Introduction to Subjective Methods
- Birth weight
- Body shape
- Weight and height
- Waist and hip circumference
- Introduction to Objective Methods
- Simple measures - stature
- Simple measures - weight
- Simple measures - circumference
- Simple measures - arm anthropometry
- Simple measures - skinfolds
- Simple measures - abdominal sagittal diameter
- Simple measures - head circumference
- Bioelectric impedance analysis
- Multi-component models
- Hydrostatic underwater weighing
- Air displacement plethysmography
- Hydrometry
- Whole body DEXA scan
- Near infrared interactance
- Whole body counting of total body potassium
- 3d photonic scan
- Magnetic resonance imaging (MRI) / Magnetic resonance spectroscopy (MRS)
- Total body electrical conductivity (TOBEC)
- Computed tomography (CT)
- Ultrasonography
- Introduction anthropometric indices
- Body mass index
- Fat and fat free mass indices
- Ponderal index
- Percentiles and Z-scores
- Anthropometry Video Resources
- Height procedure
- Protocol for measuring waist circumference
- Measuring hip circumference
- Weight and body composition procedure
Simple measures - weight
The mass (SI unit = kilogram, kg) of a body is a composite measure of total body size. It is probably the most common anthropometric measure in population health sciences, often used in the assessment of obesity.
In common usage, human body mass is often referred to as weight. In fact, weight is the force exerted on an object due to gravity (SI unit = newton, N). A measure of weight in N allows estimation of human body mass in kg using the formula W = m*g and standard gravity. In addition to the term weight often being used instead of human body mass, assessment of human body mass is also often referred to as weighing.
If conducted at multiple time points, assessment of weight provides information on an individual’s physical status, showing the amount of mass that an individual has gained or lost over time. It can be combined with a standardising variable such as age or height to produce indices that allow a simple, but crude assessment of health status, such as weight-for-height Z-scores in young children or body mass index (kg/m²) in adults. Weight assessment is also used in equations for predicting energy expenditure and in indices of body composition.
Instrumentation
A variety of scales are available for measuring weight such as beam balances and spring and digital scales. Digital scales are preferable as easier to read than scales with moving dials (see Figure A.3.4). Many digital scales, also known as body composition monitors can estimate body composition (e.g. body fat) using Bioelectrical Impedance Analysis (BIA) technology.
The scales need to be calibrated for accurate assessments of weight using standardised cast iron bar weights (see Figure A.3.5). It is common practice to carry out calibration procedures on a monthly basis. Ideally, if scales are moved on a regular basis, they should be calibrated daily.
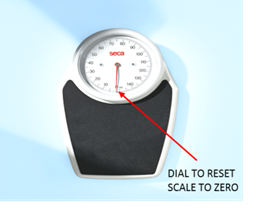
Figure A.3.4 Spring scale with a moving dial.
Source: MRC Epidemiology Unit.
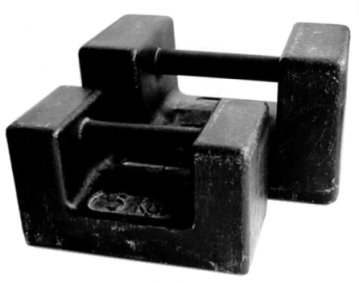
Figure A.3.5 Cast iron bar trade stamped weights for calibration use.
Source: MRC Epidemiology Unit.
Procedure:
- Weight exhibits diurnal variation, it is therefore recommended that study participants are to be measured at the same time of the day, preferably in the morning
- Ensure to clearly state the unit of the measurement e.g. metric units or Imperial scale to avoid discrepancy in recording weight. Incorrect conversion may lead to errors
- Scales should be located on a hard, even surface (not on a carpet). If measuring on carpets ensure the scale feet are inserted to prevent any rocking of the scale
In infants:
- Baby scales can be used for toddlers up to 14 kg (generally up to 2 years of age).
- Toddler over 14 kg to be weighed on sitting or standing scales as appropriate.
- Infants/toddlers should be weighed nude, without nappy (diapers). To be wrapped in a blanket to keep warm until weighing.
- Infants lie or sit (typically from 6 months) down on the scales that are designed to hold them while they are being weighed.
- Do not leave the infant unattended in any position as they may roll off or fall from the scales.
- Children over two years to be weighed in light underwear without shoes, socks and nappies if they are still wearing them. Alternatively the weight of the nappy can be subtracted from the child’s weight.
- Measurements are generally taken prior to a feed as feeding can affect the infant’s weight. A feed can add approx. 200g to an infant’s weight
- If measuring in kilograms, weight is recorded to the nearest 0.01 Kg.
- If infant/toddler is distressed, a sitting chair scale or a standing/floor scale can be used to weigh the parent/carer first then the parent/carer and child are then measured together and the previous weight is subtracted to obtain the child’s weight. However, this procedure is unreliable, partly because the adult’s weight will be recorded to the nearest 100 g.
In children and adolescents:
- If a child is 2 years old or older and will stand still, standing/floor scales can be used. However, ideally, foot print to be marked on the scale to help positioning the child in the middle of the scale. Feet to be slightly apart on the marked footprint. The procedure is the same as in adults and older individuals.
- The child or young person may require more preparation than when measuring an adult. Distraction techniques, like the use of toys, bubbles can be helpful to occupy the children. Demonstration of the procedure is important particularly in apprehensive teenagers.
Adults and older individuals:
- For routine measurement, participants should remove shoes, outer clothing such as jackets and sweaters, heavy jewellery, and contents of pockets, such as loose change, mobile phones and keys. If a higher level of precision is required, however, participants may be provided with standardised light clothing to be worn over their underwear, such as a hospital gown.
- Scales should first be ‘tared’ (reset to show a value of 0.0kg). The participant stands in the centre of the scales with arms hanging loosely by their sides. Head should be facing forward and not looking down. Once the participant is correctly positioned, the observer should wait for the scales to stabilise before recording the result to the nearest 0.1kg (if this is the chosen unit). Ideally measurement should be repeated to ensure a consistent reading.
- If measuring older individuals, help might be necessary if a person has difficulty standing. In this case, the observer will need to give extra help when the person is getting on and getting off the scale, but it is important that they do not lean on anything (including the observer) while taking the measurement.
- If the participant is missing one or more limbs, or unable to move, a sitting scale is recommended.
Assessment of weight is a fundamental anthropometric measurement and is very commonly used in a variety of health related studies. Estimation of weight is important for assessing growth and development, the construction of anthropometric indices such as weight for height, and for estimating physiological outcomes such as basal energy expenditure.
In addition to being used in isolation, weight is used in combination with other anthropometric dimensions to derive the following anthropometric indices:
- Ponderal index
- Weight for age
- Weight for height
- Weight velocity
- BMI
- BMI for age
Measurements of weight require very little data processing to derive final estimates of weight. Estimates should be quality checked during data processing in the same manner as other health related variables, for example by checking for outliers and data entry errors. There are no specific steps which are unique to weight. In some circumstances it may be necessary to convert units taken in imperial units to metric units.
An overview of weight assessment methods is outlined in Table A.3.6.
Strengths
- Inexpensive
- Limited burden to participant
- Limited burden to researcher in terms of collection and analysis
- Requires no input by participant and as such no risk of respondent biases
- Used for a wide range of indices
- Quick and easy measure when testing large groups
- Digital scales can reduce reading errors
Limitations
- Spring scales (see Figure A.3.4) may lead to reading errors as operators read off from a dial. They also need to be reset to zero before each measurements.
- Weight methods assess all body compartments, both fat and non-fat mass, and do not distinguish between them. This is important when interpreting longitudinal weight data, since any change rarely relates to fat mass only. Changes in weight correspond to changes in body water, fat, and/or lean tissue. Weight also changes with age in children as they grow and in adults as they accumulate fat.
- Body weight taken without other measures of body size is misleading because a person's weight is highly related to stature (i.e. tall people are generally heavier than short people).
- One solution to overcome the lack of specificity in weight is to use the body mass index.
Table A.3.6 Characteristics of weight assessment methods.
| Characteristic | Comment |
|---|---|
| Number of participants | Large |
| Relative cost | Low |
| Participant burden | Low |
| Researcher burden of data collection | Low |
| Researcher burden of coding and data analysis | Low |
| Risk of reactivity bias | No |
| Risk of recall bias | No |
| Risk of social desirability bias | No |
| Risk of observer bias | Yes |
| Space required | Low |
| Availability | High |
| Suitability for field use | High |
| Participant literacy required | No |
| Cognitively demanding | No |
Considerations relating to the use of weight methods in specific populations are described in Table A.3.7.
Table A.3.7 Use of weight assessment methods in different populations.
| Population | Comment |
|---|---|
| Pregnancy | Suitable. |
| Infancy and lactation | Suitable. |
| Toddlers and young children | Suitable. |
| Adolescents | Suitable. |
| Adults | Suitable. |
| Older Adults | Suitable. |
| Ethnic groups | Suitable. |
| Other | Suitable. The capacity of most of the scales commercially available is between 150-200 kg. If participants’ weight is above this, a bariatric platform with hand rails for stability can be used. It can weigh up to 500 kg. |
Factors contributing to minor weight fluctuations:
- Light clothing: is included in the weight measurement in most cases and may weigh up to 1.0kg but in most cases it weighs considerably less
- Diurnal variation: difference between food/fluid intake and bladder/bowel evacuation Source:[4]
- Diurnal variation: changes in the state of the glycogen-water pool (>0.5kg in 32% of measurements of normally-nourished men) Source:[2]
- Menstrual status: Water retention is unlikely to add more than 0.75kg in all but the most extreme cases
- Hydration status: dehydration may reduce weight by approximately 1.5% Source:[6]
Bathrooms scales are not accurate and inappropriate to use in a professional setting. In the UK, medical equipment must be approved to either the Class III or Class IV standard, depending on the intended usage. Class III scales are the default standard for medical establishments, also used in medical research.
Refer to section: practical considerations for objective anthropometry
- Scales
- Data entry form in either paper or electronic form.
- Transport suitable for moving scale to field site if necessary.
- Trained research staff
- Standard operating procedures for data collection.
- Standard operating procedures for data entry errors/extreme values/data cleaning.
- Toys (like bubbles) if measuring younger children
A method specific instrument library is being developed for this section. In the meantime, please refer to the overall instrument library page by clicking here to open in a new page.
- Duren DL, Sherwood RJ, Czerwinski SA, Lee M, Choh AC, Siervogel RM, et al. Body composition methods: comparisons and interpretation. Journal of diabetes science and technology. 2008;2(6):1139-46. Epub 2009/11/04.
- Edholm OG, Adam JM, Best TW. Day-to-day weight changes in young men. Annals of human biology. 1974;1(1):3-12. Epub 1974/01/01.
- Ismail S, Manandhar M. Better Nutrition for Older People: Assessment and Action. HelpAge International. 1999.
- Lohmann TG, Roche AF, Martorell R. Anthropometric Standardization Reference Manual Human Kinetics Books. 1988.
- Schwartz MB, Vartanian LR, Nosek BA, Brownell KD. The influence of one's own body weight on implicit and explicit anti-fat bias. Obesity. 2006;14(3):440-7. Epub 2006/05/02.
- Stevens J, Truesdale KP, McClain JE, Cai J. The definition of weight maintenance. International journal of obesity. 2006;30(3):391-9. Epub 2005/11/23.
- http://www.gosh.nhs.uk/health-professionals/clinical-guidelines/weight-measuring-childyoung-person
- http://www.who.int/childgrowth/training/module_b_measuring_growth.pdf?ua=1
