- Introduction to Subjective Methods
- Birth weight
- Body shape
- Weight and height
- Waist and hip circumference
- Introduction to Objective Methods
- Simple measures - stature
- Simple measures - weight
- Simple measures - circumference
- Simple measures - arm anthropometry
- Simple measures - skinfolds
- Simple measures - abdominal sagittal diameter
- Simple measures - head circumference
- Bioelectric impedance analysis
- Multi-component models
- Hydrostatic underwater weighing
- Air displacement plethysmography
- Hydrometry
- Whole body DEXA scan
- Near infrared interactance
- Whole body counting of total body potassium
- 3d photonic scan
- Magnetic resonance imaging (MRI) / Magnetic resonance spectroscopy (MRS)
- Total body electrical conductivity (TOBEC)
- Computed tomography (CT)
- Ultrasonography
- Introduction anthropometric indices
- Body mass index
- Fat and fat free mass indices
- Ponderal index
- Percentiles and Z-scores
- Anthropometry Video Resources
- Height procedure
- Protocol for measuring waist circumference
- Measuring hip circumference
- Weight and body composition procedure
Bioelectric impedance analysis
Bioelectrical impedance analysis (BIA) is a frequently used method for estimating body composition based on a 2-component model (2C). It measures “impedance”, the opposition to a small electrical current as it travels through the body’s water pool. Impedance comprises both resistance and reactance:
- The resistance (R) reflects the opposition of the tissue to the flow of electrons. It is related to the amount of water present in tissues.
- The reactance (Xc) by contrast reflects the capacitive losses caused by cell membranes.
The small electrical current is passed through the body from conductive surfaces or electrodes. Conductivity is higher through fat free mass (which includes muscle, bone and water) than through fat mass which contains very little water. Different body components have varying levels of impedance in response to different frequencies of the electrical current.
Output is commonly provided in the form of an impedance value (expressed in the unit Ohms, Ω; approximate range between 150Ω - 900Ω). Interpretation of the impedance value varies by BIA instrument type. For single frequency BIA, the impedance value is interpreted as resistance (R). For multi-frequency BIA and bioelectrical impedance spectroscopy, two values are provided, one for resistance (R), and one for reactance (Xc).
The impedance value is related to the volume of a conductor (the overall body size) and the square of the length of the conductor (a distance which is a function of the height of the participant). The volume of the body can be estimated from the ratio of its length/height squared divided by the resistance (H2/R, also known as the impedance index), where H is the height of the participant and R the resistance.
The impedance index is related to the volume of body water and typically used to estimate fat free mass (FFM), assuming that 73% of the body’s FFM is water. BIA is used to assess the dimensions shown in Table 1, depending upon the type of instrumentation used. The types of BIA instrument are described in more detail in the section below.
Table 1 Anthropometric dimensions which can be assessed according to BIA instrument type.
|
|
|
|
|
|---|---|---|---|
| Total fat free mass (FFM) |
|
|
|
| Total fat mass (FM) |
|
|
|
| Total body water (TBW) |
|
|
|
| Extracellular water (ECW) |
|
|
|
| Intracellular water (ICW) |
|
|
|
| Body cell mass (BMC) |
|
||
| Central and peripheral FFM and FM |
|
|
|
| Total abdominal fat and visceral fat |
|
* Multi-segmental approach only
**ViScan only
Bioelectrical impedance analysis (BIA) instruments use contact electrodes that send the electrical signal through the body. These electrodes are either patch types (similar to ECG electrodes) or stainless steel plates. BIA instruments can be broadly classified into three types: single-frequency BIA (SF-BIA); multi-frequency BIA (MF-BIA); bioelectrical impedance spectroscopy (BIS). Some BIA systems are incorporated into digital electronic scales, simultaneously measuring impedance and body weight with a force sensor.
Single-frequency BIA (SF-BIA)
SF-BIA (frequency of 50 kHz) also known as tetrapolar impedance is the most commonly used BIA instrument, based on 4 contact electrodes (2 injecting and 2 sensing electrodes). The impedance is then used together with other anthropometric data, age and gender to predict body composition variables using empirical linear regression equations.
SF-BIA is unable to distinguish the distribution of total body water into its intracellular and extracellular components.
Multi-frequency BIA (MF-BIA)
MF-BIA (frequencies up to 800 kHz) allows differentiation of intracellular and extracellular components of total body water. It relies on the principle that the body's impedance is dependent on the frequency of the alternating current applied. Total body water is distributed between the intracellular and extracellular components, separated by cell membranes. Cell membranes act as capacitors that insulate the intracellular water (ICW) at low frequencies so that predominantly extracellular water (ECW) is measured. At higher frequencies, the membranes are permeable to the current, so that ICW and ECW are both determined. MF-BIA like SF-BIA also uses regression models to evaluate FFM, TBW, ICW and ECW.
ViScan is a tetrapolar impedance method. The abdominal body composition values (total abdominal adiposity and visceral fat) are derived from extrapolation of impedance measures (at 6.25 and 50 KHz) using inbuilt algorithms and waist circumference. It consists of a wireless measurement belt and an infrared beam projected over the waist at the umbilical sagittal plane. It detects the waist circumference using two infrared sensors on either side of the base unit.
Bioelectrical impedance spectroscopy (BIS)
BIS uses a series of frequencies and it is based on the Cole–Cole plot and Hanai models which characterise the measurement segment with parallel circuits for ECW and ICW, and accounts for a capacitive effect introduced by the non-conducting membrane that separates the ICW and ECW. BIS firstly determines the electrical resistance of ECW and ICW, and then calculates the volumes of these respective components. By differentiating between extracellular water and intracellular water spaces, BIS can provide an estimate of body cell mass.
Multi-segmental approach
The multi-segmental approach which is based on 8 contact electrodes (2 on each hand and foot) assumes that the body is made up of a group of cylinders (left and right arms, the left and right legs, and the total body are measured) and provides body composition values for the trunk and limbs as well as the whole body. Multi-segmental BIA (SEG-BIA) is available in both single-frequency and multi-frequency body composition monitors.
Procedure
- Measurements should be conducted to the manufacturer’s recommendations and calibration is completed (a self-test is provided in most devices or it can be performed against an electrical resistor). Manufacturers guidelines provide calibration values cut offs.
- BIA can be performed standing or supine, via hand to foot (or arm-leg) or foot to foot (or leg-leg) impedance depending on device. Hand to foot measurements has been shown to be more accurate than foot to foot measurements. However, foot to foot impedance instruments are more user friendly for those working in the field.
- Height, weight, gender and physical activity level are typically required by the BIA instruments which then measure the resistance (in the majority of BIA devices) and reactance (for multi-frequency BIA only). Body composition estimates are then generated ‘on board’ the instrument using proprietary algorithms.
- Depending on the device, the participant lies down on a testing table and electrodes are attached to the hands and feet (Figure 1), or standing with the feet touching the electrodes of the body fat monitors (Figure 2) and if using the hand to foot 8-electrode BIA (Figure 3)
- If using the patch electrodes (ECG like electrodes) technique as in Figure 1, ensure to follow the manufacturer’s guidelines as the position of the electrodes can influence the BIA readings.
- For the ViScan, the participant is supine and the wireless measurement belt is placed directly on the skin at the umbilicus in the sagittal plane.

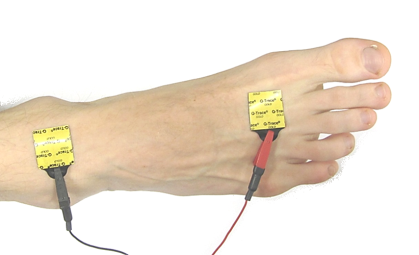
Figure 1 Electrodes placement on hand and foot.
Source: MRC Epidemiology Unit.

Figure 2 Participant’s feet touching the electrodes on a foot to foot body composition monitor.
Source: MRC Epidemiology Unit.

Figure 3 BIA using the hand to foot 8-electrode body composition monitor.
Source: MRC Epidemiology Unit.
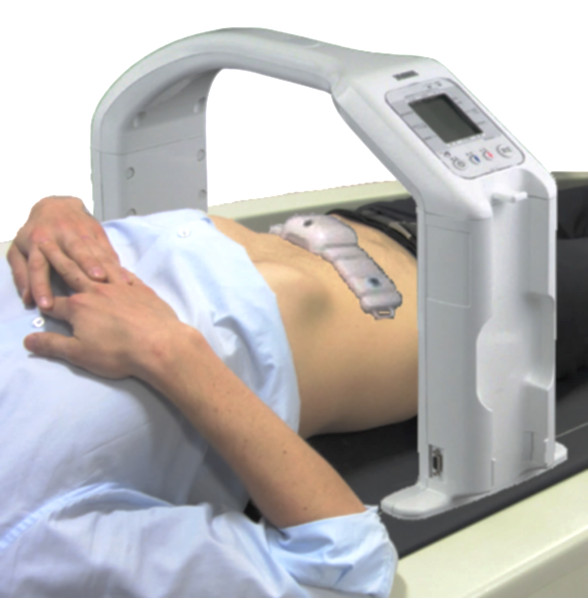
Figure 4 Estimating abdominal fat using ViScan.
Source: MRC Epidemiology Unit.
Participant instructions
Reliable BIA requires protocol standardisation and control from the following:
- Refraining from consuming caffeine (tea, coffee and energy drinks) and alcohol the day before the test (24 hour prior the test)
- Avoiding vigorous activity 8 hours before testing
- No eating or drinking within 4 hours of the test
- No diuretics within 7 days of the test
- No measurements to be carried out if participant has electrical device such as pacemaker or cochlear implant
- Shoes, socks, tights to be removed
- Hands and legs slightly separated from the body
- If skin is moist or covered with body lotion, clean the area with alcohol wipes

- BIA has been used in large-scale population studies and/or for screening purposes, where portable field methods are desirable, for the prediction of body composition.
- BIA is a reasonable method to assess and track body composition at population level but not sufficiently accurate to monitor change within an individual due to the error within the measurement.
- BIA is widely used in clinical medicine, sports medicine and weight reduction programmes.
- BIA monitors report a value of resistance (R) expressed in Ohms (Ω). If a multi-frequency device is used, a value of reactance (Xc), expressed in Ohms (Ω), is also provided.
- R, or the combination of both R and Xc, are then used in regression equations to estimate body composition together with other population characteristics such as height, weight, gender and activity levels.
- The impedance index (H2/R), reactance (Ω), age (years), sex (male = 1, female = 0) and body weight (kg) are the independent variables used in those predictions with FFM (kg) as the dependent variable.
- Most BIA instruments use in-built manufacturer prediction equations to estimate body composition variables; BIA equations generated by manufacturers are of commercial value and typically not publically available. The equations are generic and may not be applicable to specific populations. Typically instruments equations are not to be used in children under 7 years of age and in older individuals over 65 years of age.
- Numerous prediction equations of varying complexity have been published to derive body composition from BIA.
- Most BIA equations within the literature are generated from small and/or specific demographics, which restrict their use.
- Ideally in a BIA study, it is recommended to develop prediction equations and cross-validate these models against a criterion (e.g. 4-component models). However, this is not always feasible due to cost and technical constraints; therefore body composition values should be generated from published prediction equations which closely match the study population.
- When selecting a BIA prediction equation, ensure they are suitable for the device used (foot to foot vs hand to foot) and population.
- Consider the use of multiple BIA equations and then generate the average, which may help control the bias and variation inherent in the measurements.
- For the ViScan: abdominal body composition estimates are divided into total abdominal adiposity (visceral + subcutaneous fat), expressed as percentage trunk fat (range 0–75%), and visceral fat, (arbitrary units ranging from 1 to 59). The ViScan also rates these measures using arbitrary band ratings of ‘low’, ‘average’ and ‘high’ for percentage trunk fat and ‘average’, ‘high’ and ‘very high’ for visceral fat.
BIA equations
A selection of published BIA equations for predicting FFM, FM, TBW, and ECW, which include description of BIA instruments, the criterion used to validate the equations and standard error of the estimates was published by Kyle et al. (2004).
When deriving fat mass from those equations, the absolute error of estimates at individual level will vary, but the ranking of individuals (i.e. relative validity) will be relatively stable regardless of the equation used.
If, in the analysis, the investigators are only interested in determining ranking of body composition traits rather than absolute values, an alternative approach, which avoids the need for population specific validation equations can be used, as described by Vanltalie et al (1990), Tyrrell et al. (2001) and Wells et al. (2007). This method involves correcting lean and fat masses (kg) for height (cm) by deriving the following indices.
- Fat mass index = predicted fat mass (kg) / height (cm)2
- Fat free mass index = predicted fat free mass (kg) / height (cm)2
This method provides good rankings for both outcomes.
BIA data are usually expressed in the form HT2/R and then used to predict total body water. Total body water then requires adjustment for the hydration of lean tissue (HLT) to calculate lean mass. The adjustment for HLT assumes a constant level of hydration between individuals.
When using BIA data, the index for fat free mass/lean mass can be expressed as: Lean mass index = 1/R(Ω)
As lean mass is equal to total body water/hydration of lean tissue (HLT) and that total body water is proportional to H2/R, the relationship between R and lean mass index can be summarized as: Lean mass index (H2/R)/ HLT/ H2 = 1/(R*HLT)
If study population is of homogeneous age, HLT is left out as a sex specific constant, resulting in lean mass index being proportional to 1/R. Based on this theoretical approach, individuals of the same sex can be ranked according to this simple BIA index.
Further information in Wells et al. (2007).
An overview of the characteristics of BIA is outlined in Table 2.
Strengths
- Non-invasive.
- Safe to use (not recommended for participants with a pacemaker).
- Can be measured without difficulty in almost any settings.
- Limited burden to participant.
- Limited burden to researcher in terms of collection and analysis.
- Requires no input by participant and as such no risk of respondent biases.
- Quick and easy to administer.
- Easy to use.
- It can be portable.
- Reproducible.
- Relatively inexpensive.
- Minimal participant participation required.
- Estimates of body composition from BIA correlates well with those derived from other methods like DEXA.
- Multi-frequency BIA may have an added advantage over SF-BIA for evaluating leg skeletal muscle (appendicular lean mass).
- BIA is a valid and precise method for predicting body composition under controlled conditions in healthy individuals.
- In normal-weight individuals, BIS can accurately measure TBW and ECW.
- Percentage body fat by BIS is strongly correlated with a 4C model.
- High correlations between the limb impedance measured by the segmental BIA system and the appendicular lean soft tissue estimated by DXA in healthy individuals have been observed; therefore, the BIA system is able to derive measurements of this tissue.
- Total abdominal fat measured by Viscan is a good predictor of total abdominal adipose tissue measured by MRI in both lean and obese individuals.
Limitations
- It is based on the assumptions of the 2 component model.
- As the method relies upon regression equations for estimating body composition variables, BIA is only as good as the equation used.
- Published prediction equations for the estimation of FFM and % body fat show significant bias when compared to the criterion method 4C in both children and adults. In general, the equations overestimate % body fat in lean individuals and underestimate it in larger ones.
- Validity of BIA is also influenced by body size, gender, age, disease state, race or ethnicity.
- Measurements are affected by hydration status. Vigorous exercise, excessive caffeine and alcohol use (which stimulate urine production possibly leading to dehydration) will result in overestimation of fat mass.
- The disproportionality of the body in terms of shape, size and composition between limbs and trunk can affect BIA measurements.
- Poor ability to predict body fat in severely obese individuals as they tend to have higher level of body mass and water accounted by the trunk, the hydration of FFM and the ratio of ECW to ICW are also increased in obesity.
- There is a tendency for BIA to overestimate percent body fat in very lean individuals and underestimate body fat in obese participants.
- Not useful in detecting short term changes after a dietary of physical activity interventions in individuals.
- ViScan prediction of visceral fat may be limited, especially in abdominally obese individuals.
Table 2 Characteristics of bioelectric impedance analysis.
| Consideration | Comment |
|---|---|
| Number of participants | Large |
| Relative cost | Low |
| Participant burden | Low |
| Researcher burden of data collection | Low |
| Researcher burden of coding and data analysis | Low |
| Risk of reactivity bias | No |
| Risk of recall bias | No |
| Risk of social desirability bias | No |
| Risk of observer bias | No |
| Space required | Low |
| Availability | High |
| Suitability for field use | High |
| Participant literacy required | No |
| Cognitively demanding | No |
Considerations relating to the use of BIA in specific populations are described in Table 3. Estimates of body composition values are dependent on the validity of the BIA equation used for the population.
Table 3 Anthropometry by BIA in different populations.
| Population | Comment |
|---|---|
| Pregnancy | BIA may not be suitable to estimate fat-free mass FFM and fat mass FM due to the hydration status throughout pregnancy. BIA predictions will be limited in their ability to account for this variation. However, it has been used to monitor TBW changes. Some manufactures recommend not using their devices during pregnancy. |
| Infancy and lactation | There is a large variation in the different body components (water, protein, minerals) from birth to adulthood due to growth and biological maturation. This variation can significantly affect the estimate of FM and FFM, in two-compartment models like the BIA method. BIA predictions will be limited to account for these variations. Lack of valid regression equations to predict body fat make this method not suitable for these populations. However, it has been used to monitor TBW changes. Lack of standardisation of electrode placement in infants is also an issue. |
| Toddlers and young children | There is large variation in the different body components (water, protein, minerals) from birth to adulthood due to growth and biological maturation. This variation can significantly affect the estimate of FM and FFM, in two-compartment models like the BIA method. BIA predictions will be limited to account for these variations. There is lack of standardisation of electrode placement in studies. Lack of valid regression equations to predict body fat make this method not suitable for these populations Standing monitors are limited in their use in these populations as the metal electrodes are too large for children’s feet. Many of those monitors are not recommended in children below 7 years of age. |
| Adolescents | Suitable |
| Adults | Suitable |
| Older adults | Suitable, but presence of oedema may affect estimates. |
| Ethnic groups | Suitable |
| Athletes | Suitable but tend to overestimate fatness in lean individuals. |
| Other (obesity) | Suitable but tendency to underestimate fatness in those individuals. |
Refer to section: Practical considerations for objective anthropometry
- Standard operating procedures for data collection.
- Standard operating procedures for data entry errors/extreme values/data cleaning.
- Data entry form in either paper or electronic form.
- Scale to measure weight (some BIA devices can also measure weight).
- Stadiometer to measure height.
- BIA equations.
- Training of staff.
- Bohm A, Heitmann BL. The use of bioelectrical impedance analysis for body composition in epidemiological studies. Eur J Clin Nutr. 2013;67:S79-S85.
- Cheng MF, Chen YY, Jang TR, Lin WL, Chen J, Hsieh KC. Total body composition estimated by standing-posture 8-electrode bioelectrical impedance analysis in male wrestlers. Biology of sport. 2016;33(4):399-405. Epub 2017/01/17.
- Dehghan M, Merchant AT. Is bioelectrical impedance accurate for use in large epidemiological studies? Nutrition journal. 2008;7:26. Epub 2008/09/10.
- Gartner A. Reference BIA data in neonates and young infants. Nutrition. 2003;19(6):558-9. Epub 2003/06/05.
- Ghezzi F, Franchi M, Balestreri D, Lischetti B, Mele MC, Alberico S, et al. Bioelectrical impedance analysis during pregnancy and neonatal birth weight. European journal of obstetrics, gynecology, and reproductive biology. 2001;98(2):171-6. Epub 2001/09/28.
- Heymsfield SB, Lohman TG, Wang Z, Going SB. Human Body Composition, Second Edition. Windsor ON. Human Kinetics. 2005
- Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gómez JM, Heitmann BL, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AM, Pichard C; Composition of the ESPEN Working Group. Bioelectrical impedance analysis-part I: review of principles and methods. Clinical Nutrition. 2004;Oct:23(5):1226-43.
- Jebb SA, Cole TJ, Doman D, Murgatroyd PR, Prentice AM. Evaluation of the novel Tanita body-fat analyser to measure body composition by comparison with a four-compartment model. The British journal of nutrition. 2000;83(2):115-22. Epub 2000/04/01.
- Kuriyan R, Thomas T, Ashok S, Jayakumar J, Kurpad AV. A 4-compartment model based validation of air displacement plethysmography, dual energy X-ray absorptiometry, skinfold technique & bio-electrical impedance for measuring body fat in Indian adults. The Indian journal of medical research. 2014;139(5):700-7. Epub 2014/07/17.
- Silva DR, Ribeiro AS, Pavao FH, Ronque ER, Avelar A, Silva AM, et al. Validity of the methods to assess body fat in children and adolescents using multi-compartment models as the reference method: a systematic review. Revista da Associacao Medica Brasileira. 2013;59(5):475-86. Epub 2013/10/15.
- Sun SS, Chumlea WC, Heymsfield SB, Lukaski HC, Schoeller D, Friedl K, Kuczmarski RJ, Flegal KM, Johnson CL, Hubbard VS. Development of bioelectrical impedance analysis prediction equations for body composition with the use of a multicomponent model for use in epidemiologic surveys. American Journal Clinical Nutrition. 2003:77(2):331-40.
- Thomas EL, Collins AL, McCarthy J, Fitzpatrick J, Durighel G, Goldstone AP, et al. Estimation of abdominal fat compartments by bioelectrical impedance: the validity of the ViScan measurement system in comparison with MRI. Eur J Clin Nutr. 2010;64(5):525-33. Epub 2010/04/01.
- Tyrrell VJ, Richards G, Hofman P, Gillies GF, Robinson E, Cutfield WS. Foot-to-foot bioelectrical impedance analysis: a valuable tool for the measurement of body composition in children. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity. 2001;25(2):273-8. Epub 2001/06/19.
- VanItallie TB, Yang MU, Heymsfield SB, Funk RC, Boileau RA. Height-normalized indices of the body's fat-free mass and fat mass: potentially useful indicators of nutritional status. Am J Clin Nutr. 1990;52(6):953-9. Epub 1990/12/01.
- Wells JC, Fuller NJ, Dewit O, Fewtrell MS, Elia M, Cole TJ. Four-component model of body composition in children: density and hydration of fat-free mass and comparison with simpler models. Am J Clin Nutr. 1999;69(5):904-12. Epub 1999/05/08.
- Wells JC, Williams JE, Fewtrell M, Singhal A, Lucas A, Cole TJ. A simplified approach to analysing bio-electrical impedance data in epidemiological surveys. International journal of obesity. 2007;31(3):507-14. Epub 2006/08/09.
- Yamada Y, Watanabe Y, Ikenaga M, Yokoyama K, Yoshida T, Morimoto T, et al. Comparison of single- or multifrequency bioelectrical impedance analysis and spectroscopy for assessment of appendicular skeletal muscle in the elderly. Journal of applied physiology. 2013;115(6):812-8. Epub 2013/07/03.
