- Introduction to Subjective Methods
- Birth weight
- Body shape
- Weight and height
- Waist and hip circumference
- Introduction to Objective Methods
- Simple measures - stature
- Simple measures - weight
- Simple measures - circumference
- Simple measures - arm anthropometry
- Simple measures - skinfolds
- Simple measures - abdominal sagittal diameter
- Simple measures - head circumference
- Bioelectric impedance analysis
- Multi-component models
- Hydrostatic underwater weighing
- Air displacement plethysmography
- Hydrometry
- Whole body DEXA scan
- Near infrared interactance
- Whole body counting of total body potassium
- 3d photonic scan
- Magnetic resonance imaging (MRI) / Magnetic resonance spectroscopy (MRS)
- Total body electrical conductivity (TOBEC)
- Computed tomography (CT)
- Ultrasonography
- Introduction anthropometric indices
- Body mass index
- Fat and fat free mass indices
- Ponderal index
- Percentiles and Z-scores
- Anthropometry Video Resources
- Height procedure
- Protocol for measuring waist circumference
- Measuring hip circumference
- Weight and body composition procedure
Simple measures - stature
Assessment of height (or stature) is conducted by direct measurement of the length from the bottom of the feet to the highest point of the head.
Standing height can be measured in participants that can stand without assistance and who are cooperative (typically 2 to 3 years of age and older). For individuals such as infants who are unable to stand, recumbent length (also known as crown to heel length) can be measured. Alternatively, height can be inferred using equations from other measurements, such as knee height, arm-span or half-span.
Instrumentation
The instrument used to measure height varies depending upon whether it is being measured directly (i.e. standing height), measured using recumbent length, or inferred from arm-span, half-span, or knee height. In each case there are both recommended tools and alternatives which can be used if these are not available, as described in Table A.3.1.
The instrument needs to be calibrated using a standardised one-metre rod, especially when using flexible measurement tapes as these may stretch. It is common practice to carry out calibration procedures on a monthly basis.
Table A.3.1 Recommended and alternative equipment for measurement of length.
| Dimension | Recommended | Alternative |
|---|---|---|
| Stature (standing height) | Stadiometer or solid height board (in cms) with sliding head piece | Measurement tape (in cms) fixed to wall. Ruler or wood as head piece |
| Recumbent length (crown to heel length) | Recumbent length board | Measurement tape (in cms) |
| Arm-span | Steel or fibreglass measuring tape (in cms) with metal tip for placement at end of fingers | Measurement tape (in cms) |
| Half-span (demi-span) | Steel or fibreglass measuring tape (in cms) with metal tip for placement at end of fingers | Measurement tape (in cms) |
| Knee height | Broad blade sliding knee height calipers, also known as anthropometer | Measurement tape (in cms) |
Procedure: standing height
- Set up the stadiometer (or measurement tape) on a flat surface and ensure it is stable (i.e. braced against a wall), making sure that head-plate is at the top.
- The participant should remove footwear and headwear. If the participant is unable to remove the headwear, for instance due to religious reasons, measure total height with headwear, and then measure the height of the headwear. Subtract height of the headwear from total height. Record this deviation from standard measurement in a log.
- Participant should stand in the middle of the stadiometer, on the platform if there is one.
- The participant should have the back to the stadiometer:
- Feet slightly apart with back of heels touching stadiometer.
- Middle of shoulders, buttocks and back of head touching stadiometer.
- Facing straight ahead with neck straight and head in the Frankfort horizontal plane (see Figure A.3.1).
- Some participants may not be able to touch all four points against the stadiometer due to obesity or curvature of the spine. If this occurs, have the participant touching two or three of the four points of the vertical surface of the stadiometer.
- Instruct the volunteer to keep their eyes focused on a point straight ahead and to maintain an erect posture (to stand as upright/tall as he/she can).
- Lower the head-plate to the highest point of the head with enough pressure to compress the hair. Just before the measurement is taken, the participant should be instructed to inhale deeply and hold the breath, maintaining an erect posture.
- Ask the volunteer to step away ensuring that the head-plate does not move when reading off the measurement.
- Record to the nearest 0.1 cm on the measurement form. This should be done with the eye in line with the headboard.
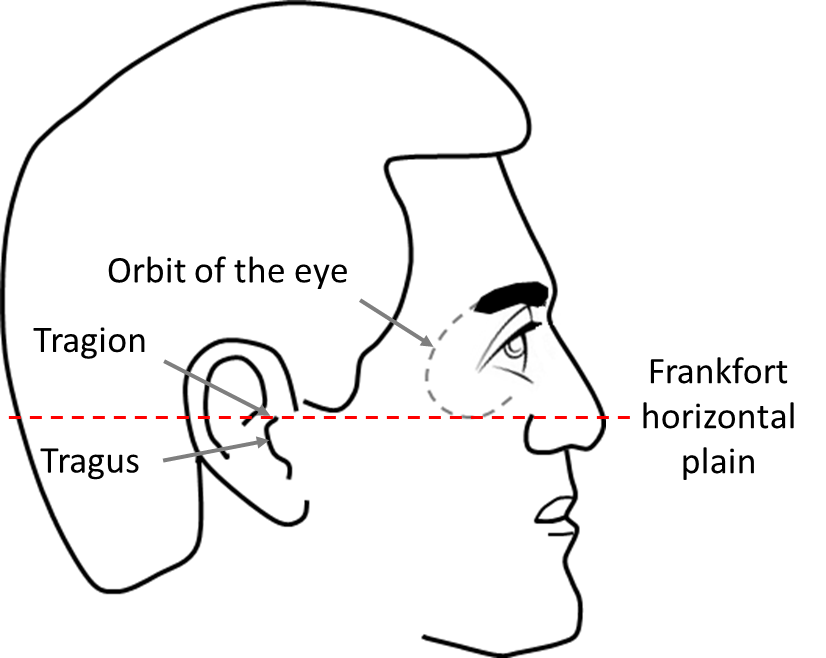
Figure A.3.1 The Frankfort horizontal plane. This plane is represented by an imaginary line between the lowest point on the margin of the orbit of the eye (the bony socket of the eye) and the tragion (the notch above the tragus, the cartilaginous projection just anterior to the external opening of the ear).
Procedure: recumbent length (crown to heel length)
Recumbent length, sometimes referred to as crown to heel length, is obtained with the participant in the supine position. It is generally reserved for children under the age of two and children under the age of three who are unable to stand without assistance.
- Find a suitable place for the device to be set up.
- Complete a visual check for any damage to the device before use.
- The area should be free of any obstruction with enough space to complete the measurement.
- Ensure that the equipment is clean.
- Explain the procedure to the parent/carer.
- Ask the parent/carer to remove child’s clothing. Ensure first that the room is warm and draft-free, do not keep the infant exposed longer than is necessary, and do not leave the child unattended in any position that they may roll from.
- Ideally two people are required for this measurement. One person positions the barefoot infant supine on the device with his/her head resting against the headboard with the neck in the midline. The child should be looking straight up in the Frankfort plane (see Figure A.3.1) and the trunk and pelvis should be aligned with the measuring device.
- The other person holds the infant’s knees together and extends them by pressing down gently, then brings the footboard up to the infant’s heels until it touches them, and reads off one accurate measurement of length to the nearest 0.1 centimeter.
Procedure: arm-span
It may not be possible to measure standing height in some participants due to curvature of the spine, weakness of back muscles or weakness in the leg muscles. In these cases, height can be estimated using arm-span. In order to do so, the participant must be able to stretch out their arms, hands and fingers in straight line (see Figure A.3.2). This measure requires two people. If only one person is present, or the participant is unable to stretch out both arms, half-span may be used instead.
- The participant should remove any bulky clothing.
- The participant should stand against a vertical surface such as a wall or door frame for support.
- Ask the participant to stretch out arms, hands and fingers with palms facing forwards. Support can be given to maintain arm position perpendicular to the body.
- The tape measure should be placed at the end of the middle finger on the right hand and held in place.
- The second measurer should then stretch out the tape across the body to the middle finger of the left hand.
- Check that the tape is horizontal to the floor.
- Take the measurement at the tip of the middle finger of the left hand.
- Record the measurement on the data entry form to the nearest 0.1 cm.
Procedure: half-span
Height can be estimated by measuring half-span for participants that are unable to stand up straight or fully outstretch both arms. This measure requires two people.
- The participant should remove any bulky clothing.
- The participant should stand against a vertical surface such as a wall or door frame for support.
- Identify the sternal notch by sliding finger from middle of chin down the throat until a bone is felt at the base of the neck. Mark this point with a soft pen which rubs off easily.
- Ask the participant to stretch out the left arm only. Hands and fingers should also be outstretched with palms facing forwards. Support can be given to maintain the arm position perpendicular to the body.
- The tape measure should be placed at the end of the middle finger on the left hand and held in place.
- The second measurer should then stretch out the tape across the body to the pen mark at the sternal notch.
- Check that the tape is horizontal to the floor.
- Take the measurement at the sternal notch.
- Record the measurement on the data entry form to the nearest 0.1 cm.
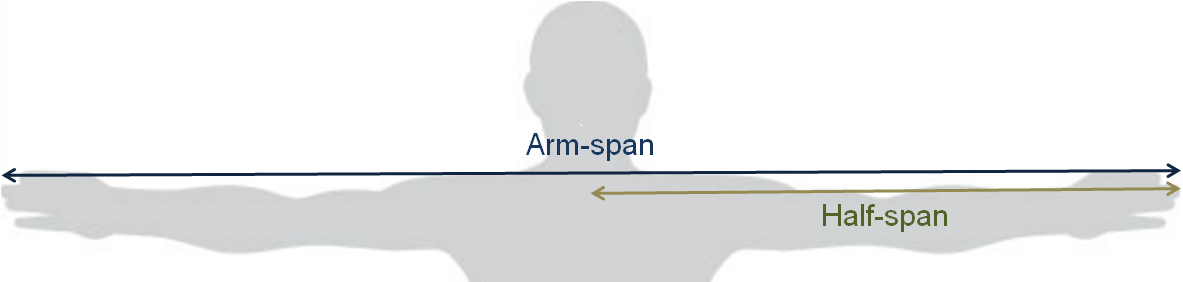
Figure A.3.2 Measurement of arm-span and half-span.
Procedure: knee height
Knee height can be used to estimate standing height in non-ambulatory participants. Measurements should be made on the left leg in order to be consistent with the leg used to derive height estimation equations.
- The participant should be lying supine with legs bare from just above the knee (see Figure A.3.3 right side). Alternatively the participant can be seated at the edge of bed/table (see Figure A.3.3 left side).
- In either position, the angles of the left knee joint and ankle should be 90 degrees and not obstructed by clothing or the surface of bed/table. Angles should be verified using right angle triangle or square.
- Place the fixed blade of the caliper under the heel of the left foot, and the moveable blade on the anterior surface of the left thigh.
- Position the caliper shaft parallel to the fibula and over the lateral malleolus , and just posterior to the head of the fibula.
- Apply gentle pressure to the fixed and moveable blades to compress the soft tissues.
- Record the measurement to the nearest 0.1 cm.
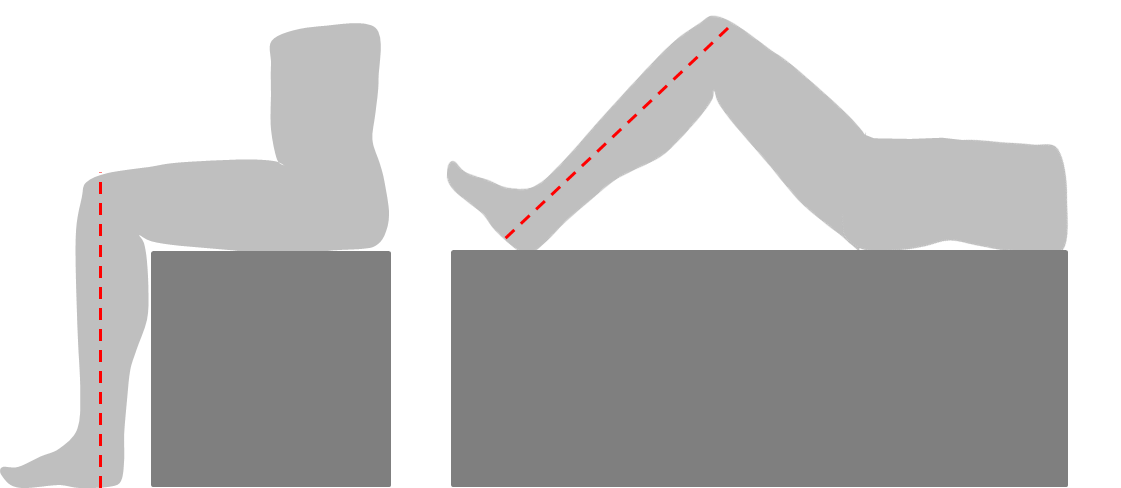
Figure A.3.3 Measurement of knee height in sitting (left) or supine positions (right).
Replicate measures
Replicate measures should be taken in all the above procedures. If two measurements are not the same, the difference between two measurements of the same participant should be calculated by subtracting the smaller value from the larger one. If the difference between two measures is greater than the largest acceptable difference for that dimension (see Table A.3.2), they should be repeated and re-checked.
Table A.3.2 Largest acceptable differences between replicate measures by dimension.
| Anthropometric dimension | Largest acceptable difference between replicate measures |
|---|---|
| Standing height | 1 cm |
| Recumbent length | 1 cm |
| Arm-span | 1 cm |
| Half-span | 0.5 cm |
| Knee height | 0.5 cm |
Assessment of height is a fundamental anthropometric measurement and is very commonly used in a variety of health related studies. Estimation of height is important for assessing growth and development, the construction of anthropometric indices such as weight for height, and for estimating physiological outcomes such as basal energy expenditure.
In addition to being used in isolation, height is used in combination with other anthropometric dimensions to derive the following anthropometric indices:
- Ponderal index
- Height for age
- Weight for height
- Height velocity
- Waist to height ratio
- BMI
- BMI for age
The steps taken to estimate height vary depending upon the type of initial raw measurement taken.
Standing height and recumbent length
Raw measures of standing height and recumbent length require very little data processing to derive final estimates of height. Estimates should be quality checked during data processing in the same manner as other health-related variables, for example by checking for outliers and data entry errors. There are no specific steps which are unique to height. In some circumstances it may be necessary to convert units taken in imperial units to metric units.
Estimation of height using arm-span, half-span and knee height
Height can be estimated from arm-span, half-span and knee height using published equations. Various equations are available, and whether or not equations are generalisable from the population in which they were derived to the population being studies should be carefully considered. Examples of equations are shown below.
Arm-span
Height can be estimated from arm-span using equations based upon the correlation between the two, which has been reported to be strong (r = 0.989). The following equation can be used to calculate height:
- Height in centimetres = (arm-span in centimetres * 0.9225) + 7.1668
However, the arm-span measurement to height relationship has been reported to be significantly different in Afro-Caribbean and Asian males. Ethnic differences should therefore be considered when making calculations. For example, separate equations have been developed for black and white women:
- Height of white women in centimeters = 29.58-(0.04 * age) + (0.81 * arm-span)
- Height of black women in centimetres = 37.72-(0.01 * age) + (0.73 * arm-span)
Half-span
Similar to the use of arm-span, half-span can also be used to estimate height. Equations which are commonly used are:
- World Health Organization: Height in meters = 0.73 * (2 x half-span) + 0.43
- Bassey et al.: Female height in centimetres = (1.35 * half-span) + 60.1
- Bassey et al.: Male height in centimetres = (1.40 * half-span) + 57.8
Knee height
Knee height can be used to estimate height using published equations, a number of which are shown in Table A.3.3.
Table A.3.3 Published equations for estimation of height from knee height.
| Population | Equation | Standard error of estimate (cm) |
|---|---|---|
| Non-Hispanic white men (U.S.) | 78.31 + (1.94 x knee height) – (0.14 x age) | 3.74 |
| Non-Hispanic black men (U.S.) | 79.69 + (1.85 x knee height) – (0.14 x age) | 3.80 |
| Mexican-American men (U.S.) | 82.77 + (1.83 x knee height) – (0.16 x age) | 3.68 |
| Non-Hispanic white women (U.S.) | 82.21 + (1.85 x knee height) – (0.21 x age) | 3.98 |
| Non-Hispanic black women (U.S.) | 89.58 + (1.61 x knee height) – (0.17 x age) | 3.82 |
| Mexican-American women (U.S.) | 84.25 + (1.82 x knee height) – (0.26 x age) | 3.77 |
| Taiwanese men | 85.10 + (1.73 x knee height) – (0.11 x age) | 3.86 |
| Taiwanese women | 91.45 + (1.53 x knee height) – (0.16 x age) | 3.79 |
| Elderly Italian men | 94.87 + (1.58 x knee height) – (0.23 x age) + 4.8 | 4.30 |
| Elderly Italian women | 94.87 + (1.58 x knee height) – (0.23 x age) | 4.30 |
| French men | 74.7 + (2.07 x knee height) – (-0.21 x age) | 3.80 |
| French women | 67.00 + (2.2 x knee height) – (0.25 x age) | 3.50 |
| Mexican men | 52.6 + (2.17 x knee height) | 3.31 |
| Mexican women | 73.70 + (1.99 x knee height) – (0.23 x age) | 2.99 |
| Filipino Men | 96.50 + (1.38 x knee height) – (0.08 x age) | |
| Filipino women | 89.63 + (1.53 x knee height) – (0.17 x age) | |
| Malaysian men | (1.924 x knee height) + 69.38 | 3.51 |
| Malaysian women | (2.225 x knee height) + 50.25 | 3.40 |
Adapted from: mna-elderly.com
An overview of height methods is outlined in Table A.3.4.
Strengths
- Inexpensive.
- Limited burden to participant.
- Limited burden to researcher in terms of collection and analysis.
- Requires no input by participant and as such no risk of respondent biases.
- Used for a wide range particularly indices.
Limitations
- Equations used to predict height from arm-span, half-span and knee height may not be generalisable between populations.
- It may be difficult to measure height or one of its proxies in particularly frail individuals.
- Estimates of height using different instruments and estimation equations may not be comparable.
Table A.3.4 Characteristics of height methods.
| Characteristic | Comment |
|---|---|
| Number of participants | Large |
| Relative cost | Low |
| Participant burden | Low |
| Researcher burden of data collection | Low |
| Researcher burden of coding and data analysis | Low |
| Risk of reactivity bias | No |
| Risk of recall bias | No |
| Risk of social desirability bias | No |
| Risk of observer bias | Yes |
| Space required | Low |
| Availability | High |
| Suitability for field use | High |
| Participant literacy required | No |
| Cognitively demanding | No |
Considerations relating to the use of height methods in specific populations are described in Table A.3.5.
Table A.3.5 Use of height methods in different populations.
| Population | Comment |
|---|---|
| Pregnancy | May be difficult for participant to stand directly against stadiometer. May require estimation of height using arm-span, half-span, or knee height. |
| Infancy and lactation | Recumbent length should be used in place of standing height. |
| Toddlers and young children | Recumbent length may be used if participant cannot stand unaided or is uncooperative. |
| Adolescents | |
| Adults | |
| Older Adults | It may be difficult for older individuals to stand up straight due to curvature of the spine, weakness of back muscles and weakness in the leg muscles. |
| Ethnic groups | There may be ethnicity dependent differences in the relationships between height and proxy measures such as knee height, half-span and arm-span. |
| Other | Wearing of religious head-wear may impede measurement. Measure height with head-wear, and then subtract the measurement of the height of the head-wear. Record this deviation from standard measurement. |
- Height can vary throughout the day and should therefore be measured at approximately the same time each day.
- Equipment performance to be assessed as part of a quality control program. This can also be arranged with the manufacturers.
- For all the anthropometric measurements, it is recommended to carry our quality control workshops, where the intra and inter observer errors are assessed to monitor reliability of these measures.
Refer to section: practical considerations for objective anthropometry
- Stadiometer; or solid height board (in cms) with sliding head-plate; or measurement tape (in cms) fixed to a wall with a ruler or wood as the head-plate.
- Data entry form in either paper or computerised form.
- Transport suitable for moving stadiometer to field site if necessary.
- Trained research staff, two required for certain measures.
- Standard operating procedures for data collection.
- Standard operating procedures for data entry errors/extreme values/data cleaning.
A method specific instrument library is being developed for this section. In the meantime, please refer to the overall instrument library page by clicking here to open in a new page.
- Bassey EJ. Demi-span as a measure of skeletal size. Annals of human biology. 1986;13(5):499-502. Epub 1986/09/01.
- Cheng HS, See LC, Shieh YH. Estimating stature from knee height for adults in Taiwan. Chang Gung medical journal. 2001;24(9):547-56. Epub 2001/12/01.
- Chumlea WC, Guo SS, Steinbaugh ML. Prediction of stature from knee height for black and white adults and children with application to mobility-impaired or handicapped persons. Journal of the American Dietetic Association. 1994;94(12):1385-8, 91; quiz 9-90. Epub 1994/12/01.
- Chumlea WC, Guo SS, Wholihan K, Cockram D, Kuczmarski RJ, Johnson CL. Stature prediction equations for elderly non-Hispanic white, non-Hispanic black, and Mexican-American persons developed from NHANES III data. Journal of the American Dietetic Association. 1998;98(2):137-42. Epub 2003/01/08.
- De Lucia E, Lemma F, Tesfaye F, Demisse T, Ismail S. The use of armspan measurement to assess the nutritional status of adults in four Ethiopian ethnic groups. Eur J Clin Nutr. 2002 Feb;56(2):91-5.
- Donini LM, de Felice MR, de Bernardini L, Ferrari G, Rosano A, de Medici M, et al. Prediction of stature in the Italian elderly. The journal of nutrition, health & aging. 2000;4(2):72-6. Epub 2000/06/08.
- Ismail S. and Manandhar M. Better Nutrition for Older People: Assessment and Action. Helpage International. 1999. ISBN: 1 872590 40 3
- Jarzem PF, Gledhill RB. Predicting height from arm measurements. Journal of pediatric orthopedics. 1993;13(6):761-5. Epub 1993/11/01.
- Mendoza-Nunez VM, Sanchez-Rodriguez MA, Cervantes-Sandoval A, Correa-Munoz E, Vargas-Guadarrama LA. Equations for predicting height for elderly Mexican Americans are not applicable for elderly Mexicans. American journal of human biology : the official journal of the Human Biology Council. 2002;14(3):351-5. Epub 2002/05/10.
- Organization WH. Management of severe malnutrition: a manual for physicians and other senior health workers. Geneva: World Health Organization. 1999.
- Reeves SL, Varakamin C, Henry CJ. The relationship between arm-span measurement and height with special reference to gender and ethnicity. European journal of clinical nutrition. 1996;50(6):398-400. Epub 1996/06/01.
- http://www.mna-elderly.com/forms/mna_guide_english_sf.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1545095/pdf/archdisch00801-0068.pdf
