- What is physical activity?
- Energy expenditure
- Movement
- Posture
- Volume, intensity, duration, frequency
- Physical behaviour type
- Contextual information: Domain, spatial settings and social contexts
- Sedentary behaviour
- Physical activity guidelines
- Physical activity variation
- Inventory and taxonomy of pattern metrics
- Introduction to objective methods
- Pedometers
- Accelerometers
- Heart rate monitors
- Combined heart rate and motion sensors
- Direct observation
- Doubly labelled water
- GPS and other GNSS receivers
- Multi sensor monitors
- Harmonisation of physical activity data
- Case study: Physical activity during pregnancy and anthropometry of the offspring
- Comparison of three harmonisation methods using validation data
- Network harmonisation of physical activity data using validation data
- Physical Activity Assessment Video Resources
- Getting participants started with the Axivity Monitor
- Wearing the Axivity Monitor
- Getting participants started with the ActiGraph Monitor
- Getting participants started with the Actiheart Monitor
- Wearing the ActiGraph monitor
- Step Test Procedure
Heart rate monitors
Heart rate increases with metabolic demand for oxygen and is an indirect indicator of physical activity. Measurement of heart rate can be used to estimate physical activity intensity or energy expenditure (EE) assuming a linear relationship between heart rate and EE (or oxygen consumption, VO2).
This method is limited by considerable inter-individual variation and, to a lesser extent, intra-individual variation in the heart rate-to-EE relationship (Li et al., 1993). Heart rate at a given physical activity intensity will not be the same between most individuals due to differences in age, gender, movement economy, and physical fitness. Heart rate can also be affected by factors other than physical activity, such as ambient temperature, dehydration, illness or emotional stress. The relative influence from these factors is greatest during low intensity and sedentary behaviours. As a result, assessment of physical activity using heart rate is best at moderate and vigorous intensity levels and least accurate at lower intensity levels.
Various techniques have been developed to overcome these limitations, including the use of individual calibration of the relationship between heart rate and EE to address the issue of inter-individual variation, and the FLEX heart rate method to limit the impact of non-activity influences on the energy estimate. Heart rate monitors can provide minute-by-minute and beat-by-beat information relating to the pattern of physical activity in terms of duration, frequency and intensity. Estimates of EE and physical activity intensity depend upon how estimates are derived and the level of individual calibration (Brage et al., 2007; Schrack et al., 2012). The dimensions of physical activity assessed by heart rate monitoring are described in Table P.3.9.
Table P.3.9 The physical activity dimensions which can be assessed by heart rate monitor.
| Dimension | Possible to assess? |
|---|---|
| Duration | ✔ |
| Intensity | ✔ |
| Frequency | ✔ |
| Volume | ✔ |
| Total physical activity energy expenditure | ✔ |
| Type | |
| Timing of bouts of activity (i.e. pattern of activity) | ✔ |
| Domain | |
| Contextual information (e.g. location) | |
| Posture | |
| Sedentary behaviour | ✔ |
Electrocardiography (ECG) based heart rate monitors measure the electrical potential on the surface of the skin using electrodes attached to the chest (see Figure P.3.8). This results in a voltage time-series signal, which may be stored as the full ECG waveform (as used in Holter monitoring) for offline processing, or may be processed by the monitor’s inbuilt peak detection algorithm to identify heart beats (the QRS complex in the cardiac cycle). Data are then stored as inter-beat interval time-series (in milli-seconds) or may be further reduced to average heart rate values, for example number of beats every minute. This final step usually employs a degree of filtering to limit the impact of missed and/or ectopic beats. There are therefore three steps involved in deriving a robust estimate of average heart rate; one measurement step and two inference steps.
Optical heart rate monitors work on a different principle of measurement, namely by detecting the fluctuation in blood perfusion of the skin (finger, wrist, earlobe) that occurs during the cardiac cycle by differential absorption of light from a LED to a photodiode (photoplethysmography, PPG); the subsequent inferential steps of deriving heart rate in beats per minute are similar in principle to those performed on the ECG signal (peak detection to derive beats, followed by filtering to get a robust average heart rate estimate).
The development of heart rate monitors with internal memory capacity for storing multiple days’ of data in high time resolution has increased the feasibility of this objective measure of physical activity; some do not have visual display of heart rate which further improves feasibility (reduces re-activity) for observational research.
There are a wide range of heart rate monitors which vary in sophistication but in practical terms there are three main types of heart rate monitors used to measure physical activity in population health research:
- Chest strap (see Figure P.3.8) which is wirelessly connected to a data logger stored in a watch or directly on the device itself. The chest strap measures the ECG and has at least two electrodes which are moistened and securely fastened to the lower chest. The chest strap must be tightly fitted to ensure good contact with the skin and this can be uncomfortable for the participant, who may be asked to wear the device during several days of free-living. The Polar Vantage XL, Polar Accurex II and Accumen Basix Performance are examples of this configuration (Terbizan et al., 2002).
- Single-device measuring the ECG and clipping onto two or more sticky ECG electrodes, a method commonly used to evaluate patients for cardiac conditions (Holter monitoring). When using this method, it is advised to provide extra electrodes and instructions for replacing these to avoid issues with monitor placement and skin irritation. The CamNtech Actiheart is one example of this configuration (Brage et al., 2015).
- Optical device based on photoplethysmography, typically worn on the wrist or a finger. This is a more recent technological development and has been less used in population research; however wearing devices on the wrist usually has very high participant tolerance. Examples include Apple Watch, Garmin, Scosche Rhythm, Mio Alpha, Fitbit Charge HR, Basis Peak, Microsoft Band, and TomTom Runner Cardio (Stahl et al., 2016; Henriksen et al., 2018). An example of finger-based heart rate monitoring is the Oura Ring.
Figure P.3.8 Wear location of a heart rate monitor chest strap.
Calibration procedures
There are two key issues associated with the use of heart rate to estimate physical activity:
- The linear relationship between heart rate and EE does not hold at low intensity physical activity.
- There is considerable inter-individual variation in the relationship between heart rate and EE
Due to inter-individual variability of an individual’s heart rate response to activity, individual calibration is required to increase the accuracy of heart rate data to estimate physical activity (Brage et al., 2007).
This typically includes collection of heart rate response to a submaximal exercise protocol with a known or measured EE cost profile. The relationship derived between observed heart rate and EE during the exercise test is then applied to predict EE in free-living situations. Determining whether to individually calibrate or not (and how) is a matter of weighing up the likely increased validity of the measurement versus the feasibility of the calibration method.
There are different options for calibration. The most intensive methods are likely to produce more precise estimates but may be perceived as more invasive, take more time for the participant to undertake in the laboratory setting, and are therefore not always feasible for large-scale studies. Exercise protocols for establishing heart rate to EE relationships can also be risk-stratified (Gonzales et al., 2021). The choice of calibration method needs to take into account the characteristics of the population being studied and secondly the settings under which a calibration test could be carried out. If necessary existing exercise tests can be adapted or new ones developed for a specific application; the underlying principle is the same in that heart rate data over a reasonable intensity range are needed. Examples of different approaches to individual calibration in descending order of validity but ascending order of feasibility are:
- Wide-range graded ergometer test with EE measurement
- Wide-range graded ergometer test with estimated EE profile
- Moderate-range graded step test with EE measurement
- Moderate-range graded step test with estimated EE profile
- Low-range walk test with EE measurement
- Low-range walk test with estimated EE profile
- No dynamic calibration (using only resting heart rate)
The choice of calibration protocol and in particular its intensity range will affect the accuracy of the prediction of EE for each heart rate level (Corder et al., 2008). Simplified methods, such as walk or step tests or even no dynamic calibration but simply using resting heart rate and other possible proxy indicators of fitness (age, sex) have been suggested, accepting the reduction in precision (Brage et al., 2007; Corder et al., 2005).
Simple methods such as the 8-minute ramped step test with a 2-minute recovery are portable and quick, making them feasible for field studies involving larger numbers of people or where facilities are minimal. The use of only sleeping heart rate is an alternative calibration method and measurements taken overnight explain some variation in the heart rate and EE relationship without the need for resource-demanding calibration procedures but it is not as good as a dynamic test (Brage et al., 2007). The relationship between the validity and feasibility of different calibration procedures is demonstrated by Figure P.3.9.
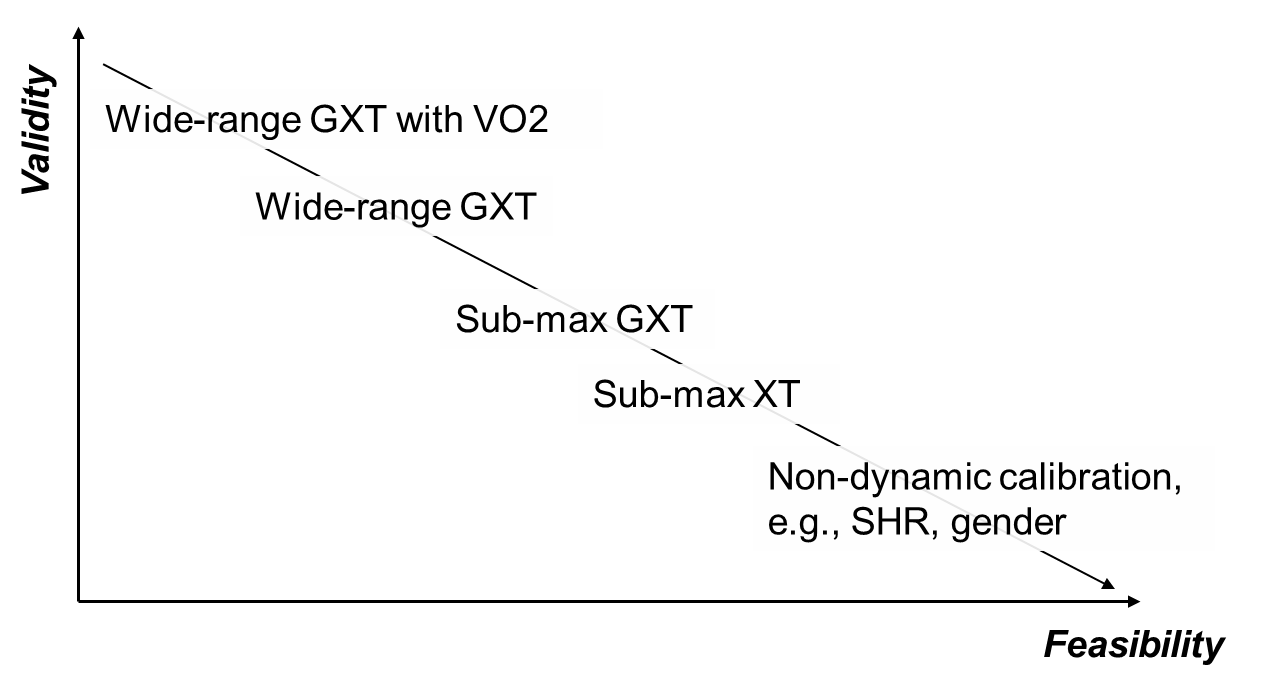
Figure P.3.9 Trade-off between validity and feasibility of calibration procedures. Adapted from: Brage et al., 2007.
GXT: graded exercise test; XT: exercise test; SHR: sleeping heart rate.
Heart rate monitoring is used when estimates of physical activity energy expenditure (PAEE) and time spent in moderate and vigorous intensity physical activity are required. The method also provides estimates of frequency, duration, and timing of these activities. The need for individual calibration for achieving better accuracy may limit use of this method for some larger studies (Armstrong et al., 2006) although several larger cohorts have done so (Lindsay et al., 2019; Wareham et al. 1997).
It should be noted that accuracy is considerably improved by using individual calibration; this is particularly important for interventions that may have altered fitness, since estimates of PAEE and time spent in different intensities of activity may otherwise be differentially biased with respect to intervention group.
Using group-based calibration equations (rather than individual calibration) reduces accuracy but increases the feasibility of the method as an objective measure of physical activity in larger epidemiological studies where conducting individual calibration tests would be prohibitive. Improvements in user acceptability, for example via more skin-friendly materials for ECG pads or wrist-based photoplethysmography technology, as well as statistical techniques for inference of true heart rate from potentially noisy measurements of heart rate (Stegle et al., 2008) would make this method more applicable to very large studies with >100,000 individuals. The Apple Heart Study used the optical measurement of heart rate from Apple watches to detect atrial fibrillation in >400,000 individuals (Perez et al, 2019).
Flex heart rate method
Heart rate monitoring is used when estimates of physical activity energy expenditure (PAEE) and time spent in moderate and vigorous intensity physical activity are required. The method also provides estimates of frequency, duration, and timing of these activities.
Individual assessment of resting energy expenditure and resting heart rate, as well as an exercise test linking heart rate changes to different energy expenditure levels is required.
TEE = EE sleep + EE rest + EE physical activity
EE sleep = BMR
EE rest = REE (for time when HR < FLEX HR)
EE physical activity = EE from regression equation (for time when HR ≥ FLEX HR)
The heart rate Flex point is defined empirically as the average of the lowest heart rate during exercise and the highest during rest (Ceesay et al., 1989). Livingstone et al. (1992) evaluated the accuracy of the Flex heart rate method to estimate TEE in 36 free-living children using DLW. Individual differences ranged from -16.7% to 18.8%; mean group differences ranged from -9.2% ± 4.5% to 3.5% ± 6.6%. The method has also been validated in various adult populations comparing EE estimates with those measured by whole body calorimetry and DLW. Recent estimates from UK adults were reported to agree with DLW-based estimates of PAEE and TEE with no significant bias irrespective of individual calibration level but with higher accuracy and correlations (range r=0.66-0.76 for TEE) for calibrated estimates (Ceesay et al., 1989; Ekelund et al., 2002; Livingstone et al., 1990; Brage et al., 2015).
Limitations of the Flex heart rate method
The key limitations of the Flex heart rate method are that it depends on the assumption that the measured heart rate - EE relationship is reliable in free-living daily activities and that it reflects cardiorespiratory responses to physical activity, but not other physiological responses to external stimuli e.g. caffeine or emotional stress.
The individual calibration should be undertaken as close to the heart rate monitoring period as possible since the estimation of energy expenditure is based on the assumption that the measured heart rate - EE relationship is representative for the physiological state of the individual during the monitoring period. This relationship may change as a result of improved cardiorespiratory fitness, changes in body composition or certain conditions/diseases (e.g. anaemia).
Other modelling approaches
The feasibility of using heart rate monitoring without individual calibration to estimate EE using prediction parameters has been investigated and found suitable for ranking individuals in epidemiological studies (Rennie et al., 2001). Other studies have also shown that it is possible to estimate EE from heart rate using multivariate predictive equations derived from group data in adults (Hiilloskorpi et al., 2003; Dugas et al, 2005; Keytel et al., 2005; Strath et al., 2000) and children (Livingstone et al., 2000).
Variation in applying different prediction equations has been investigated and individual differences found; group level analysis was found to be satisfactory for some population groups (Iannotti et al., 2004). It is important that prediction equations are derived in studies with adequate numbers (>100) and are representative of the population to be studied. Another approach to analysing heart rate data has been to adjust for fitness and age to increase the validity of using heart rate to predict EE (Strath et al., 2000).
Absolute heart rate indices
Absolute heart rate values have also been used to distinguish between activity intensities (Sirard & Pate, 2001), albeit less frequently. The method is based on using a heart rate above a certain threshold, e.g. ≥140 beats per minute, as an approximate measure of moderate-vigorous physical activity (MVPA) in children (Simons-Morton et al., 1990).
Relative heart rate indices
A common method to derive relative heart rate indices utilises a measurement of the individual’s resting heart rate (RHR) or expressing heart rate relative to (usually predicted) maximal heart rate. Four of the most commonly used heart rate indices are:
- Net heart rate: Absolute heart rate minus resting heart rate (Andrews, 1971; Brage et al., 2007), e.g. reported as mean across the day.
- Activity heart rate ratio (AHRR)-25: Binary indicator of intensity defined as heart rate >25% above resting heart rate (ratio HR/RHR>1.25). Daily estimates may be reported as proportion of monitored time spent above this level (Assah et al., 2008).
- Activity heart rate ratio (AHRR)-50: Binary indicator of intensity defined as heart rate 50% above resting heart rate (ratio HR/RHR>1.50). Daily estimates reported as proportion of time above this level.
- Percentage maximum heart rate: Absolute heart rate divided by age-predicted max heart rate.
The impact of differences in the definition of resting heart rate and how it is measured on the estimation of physical activity has been demonstrated (Logan et al., 2000).
An overview of the characteristics of heart rate monitoring is outlined in Table P.3.10.
Chest strap monitors must be well fitted in order to provide contact with the skin; this may be uncomfortable when measuring heart rate over several days. Alternatively ECG electrodes can be used to obtain heart rate, however these can also be difficult to wear over longer periods due to problems with placement and skin irritation (Andre & Wolf, 2007).
Strengths
- Suitable for most populations
- Low respondent burden for short wearing times
- Easy and quick for data collection
- Non wearing time easily identified
- Waterproof
- Relatively cheap
- Physical activity may be measured at group level
- Linear relationship between heart rate and EE at moderate-to-vigorous intensity activity
Limitations
- Relationship between heart rate and EE at low levels of activity is not strong so it will not provide an accurate estimate of activity at this intensity.
- A degree of individual calibration is required.
- Heart rate response tends lag after changes in movement and remain elevated after movement stops; this means that heart rate may mask sporadic activity; this is of particular relevance in children (Trost, 2007).
- Factors other than physical activity affect HR:
- Anxiety or emotional stress, fear or excitement
- Ambient temperature which may be an issue in hot climates
- Caffeine and some recreational drugs
- High dose of beta blockers is a contraindication to the method
- Participant burden increases over longer periods
- Electrodes or chest straps may cause discomfort
- Not always easy to pick up heart rate, due to interference from household devices (telemetry systems) or a bad connection with the skin or other sources of noise which will have to be considered during data cleaning
Table P.3.10 Characteristics of heart rate monitoring.
| Consideration | Comment |
|---|---|
| Number of participants | Small to very large |
| Relative cost | Moderate |
| Participant burden | High with individual calibration |
| Researcher burden of data collection | High with individual calibration |
| Researcher burden of data analysis | High |
| Risk of reactivity bias | Yes |
| Risk of recall bias | No |
| Risk of social desirability bias | No |
| Risk of observer bias | No |
| Participant literacy required | No |
| Cognitively demanding | No |
Considerations relating to the use of heart rate monitors for assessing physical activity are summarised by population in Table P.3.11.
Table P.3.11 Physical activity assessment by heart rate monitor in different populations.
| Population | Comment |
|---|---|
| Pregnancy | Suitable. PPG-based methods likely more accepted. |
| Infancy and lactation | Not suitable. |
| Toddlers and young children | May have difficulty wearing electrodes and chest strap both in terms of having more sensitive skin but also the size of straps and belts of the monitors themselves. There are also small pieces which could be swallowed. Child curiosity could lead to fiddling which interferes with heart rate signal. |
| Adolescents | Suitable. |
| Adults | Suitable. |
| Older Adults | Generally suitable. Safety may be a concern when conducting exercise testing for individual calibration. Self-paced protocols may be viable alternatives. Dexterity may be an issue when changing electrodes/placing device. |
| Ethnic groups | Generally suitable. PPG accuracy may be lower on darker skin. |
| Other | In obese individuals it may be more difficult to get a good heart rate signal due to adiposity attenuating the signal. |
- Participant screening may be necessary to ensure health prior to exercise test used for individual calibration
- Instructions on monitor placement and wearing plus contact details should be supplied
- Participants can be contacted by phone, SMS or email during the planned assessment to encourage compliance
- Individuals may not wish to wear a chest strap or ECG electrodes; the method may not be suitable for use in very young children
- Choose an individual calibration protocol suitable for environment/facilities and that participants will be used to, for example lack of experience on a treadmill may cause additional stress leading to inaccurate representation of workload to heart rate; self-paced over-ground walking or running or an exercise bike test may work better in these circumstances
- People with sensitive skin may experience skin irritation when wearing ECG electrodes
- A monitor with display of heart rate on a wrist device may influence behaviour (reactivity), especially on the first day of wear
- If reactivity is suspected, data from first day of wear can be compared with subsequent days and either scaled down or excluded
- Heart rate monitors and a range of different sized chest straps (if system comprises chest straps)
- A range of hypoallergenic ECG electrodes, suitable for long periods of wear (if system comprises ECG electrodes)
- The level of calibration will determine equipment required; at its most intensive calibration level, it requires a treadmill (or other ergometer) and a respiratory gas analyser
- At a lower level of calibration a step or a measured distance for a timed walk test may be used
- Processing of heart rate data requires considerable researcher time and ideally dedicated computer programming
A list of specific heart rate monitoring instruments is being developed for this section. In the meantime, please refer to the overall instrument library page by clicking here to open in a new page.
- Andre D, Wolf DL. Recent advances in free-living physical activity monitoring: a review. Journal of Diabetes Science and Technology. 2009;1:760-7
- Andrews RB. Net heart rate as a substitute for respiratory calorimetry. The American Journal of Clinical Nutrition. 1971;24:1139-47
- Armstrong N, Welsman JR. The physical activity patterns of European youth with reference to methods of assessment. Sports Medicine (Auckland, N.Z.). 2006;36:1067-86
- Assah FK, Brage S, Ekelund U, Wareham NJ. The association of intensity and overall level of physical activity energy expenditure with a marker of insulin resistance. Diabetologia. 2008;51:1399-407
- Brage S, Ekelund U, Brage N, Hennings MA, Froberg K, Franks PW, Wareham NJ. Hierarchy of individual calibration levels for heart rate and accelerometry to measure physical activity. Journal of Applied Physiology (Bethesda, Md.:1985). 2007;103:682-92
- Brage S, Brage N, Franks PW, Ekelund U, Wareham NJ. Reliability and validity of the combined heart rate and movement sensor Actiheart. European Journal of Clinical Nutrition. 2005;59:561-70
- Brage S, Westgate K, Franks PW, Stegle O, Wright A, Ekelund U, Wareham NJ. Estimation of Free-Living Energy Expenditure by Heart Rate and Movement Sensing: A Doubly-Labelled Water Study. PLOS ONE. 2015;10:e0137206
- Ceesay SM, Prentice AM, Day KC, Murgatroyd PR, Goldberg GR, Scott W, Spurr GB. The use of heart rate monitoring in the estimation of energy expenditure: a validation study using indirect whole-body calorimetry. The British Journal of Nutrition. 1989;61:175-86
- Corder K, Brage S, Wareham NJ, Ekelund U. Comparison of PAEE from combined and separate heart rate and movement models in children. Medicine and Science in Sports and Exercise. 2005;37:1761-7
- Corder K, Brage S, Mattocks C, Ness A, Riddoch C, Wareham NJ, Ekelund U. Comparison of two methods to assess PAEE during six activities in children. Medicine and Science in Sports and Exercise. 2007;39:2180-8
- Corder K, Ekelund U, Steele RM, Wareham NJ, Brage S. Assessment of physical activity in youth. Journal of Applied Physiology (Bethesda, Md.:1985). 2008;105:977-87
- Dugas LR, van der Merwe L, Odendaal H, Noakes TD, Lambert EV. A novel energy expenditure prediction equation for intermittent physical activity. Medicine and Science in Sports and Exercise. 2005;37:2154-61
- Ekelund U, Yngve A, Westerterp K, Sjöström M. Energy expenditure assessed by heart rate and doubly labeled water in young athletes. Medicine and Science in Sports and Exercise. 2002;34:1360-6
- Gonzales TI, Westgate K, Strain T, Hollidge S, Jeon J, Christensen DL, Jensen J, Wareham NJ, Brage S. Cardiorespiratory fitness assessment using risk-stratified exercise testing and dose-response relationships with disease outcomes. Scientific Reports. 2021;11:15315
- Hiilloskorpi HK, Pasanen ME, Fogelholm MG, Laukkanen RM, Mänttäri AT. Use of heart rate to predict energy expenditure from low to high activity levels. International Journal of Sports Medicine. 2003;24:332-6
- Henriksen A, Haugen Mikalsen M, Woldaregay AZ, Muzny M, Hartvigsen G, Hopstock LA, Grimsgaard S. Using Fitness Trackers and Smartwatches to Measure Physical Activity in Research: Analysis of Consumer Wrist-Worn Wearables. Journal of Medical Internet Research. 2017;20:e110
- Iannotti RJ, Claytor RP, Horn TS, Chen R. Heart rate monitoring as a measure of physical activity in children. Medicine and Science in Sports and Exercise. 2004;36:1964-71
- Keytel LR, Goedecke JH, Noakes TD, Hiiloskorpi H, Laukkanen R, van der Merwe L, Lambert EV. Prediction of energy expenditure from heart rate monitoring during submaximal exercise. Journal of Sports Sciences. 2005;23:289-97
- Kowalski K, Rhodes R, Naylor PJ, Tuokko H, MacDonald S. Direct and indirect measurement of physical activity in older adults: a systematic review of the literature. The International Journal of Behavioral Nutrition and Physical Activity. 2011;9:148
- Leonard WR. Measuring human energy expenditure: what have we learned from the flex-heart rate method? American Journal of Human Biology : the official journal of the Human Biology Council. 2003;15:479-89
- Li R, Deurenberg P, Hautvast JG. A critical evaluation of heart rate monitoring to assess energy expenditure in individuals. The American Journal of Clinical Nutrition. 1993;58:602-7
- Lindsay T, Westgate K, Wijndaele K, Hollidge S, Kerrison N, Forouhi N, Griffin S, Wareham N, Brage S. Descriptive epidemiology of physical activity energy expenditure in UK adults (The Fenland study). The International Journal of Behavioral Nutrition and Physical Activity. 2019;16:126
- Livingstone MB, Prentice AM, Coward WA, Ceesay SM, Strain JJ, McKenna PG, Nevin GB, Barker ME, Hickey RJ. Simultaneous measurement of free-living energy expenditure by the doubly labeled water method and heart-rate monitoring. The American Journal of Clinical Nutrition. 1990;52:59-65
- Livingstone MB, Coward WA, Prentice AM, Davies PS, Strain JJ, McKenna PG, Mahoney CA, White JA, Stewart CM, Kerr MJ, et al. Daily energy expenditure in free-living children: comparison of heart-rate monitoring with the doubly labeled water (2H2(18)O) method. The American Journal of Clinical Nutrition. 1992;56:343-52
- Livingstone MB, Robson PJ, Totton M. Energy expenditure by heart rate in children: an evaluation of calibration techniques. Medicine and Science in Sports and Exercise. 2000;32:1513-9
- Logan N, Reilly JJ, Grant S, Paton JY. Resting heart rate definition and its effect on apparent levels of physical activity in young children. Medicine and Science in Sports and Exercise. 2000;32:162-6
- Perez MV, Mahaffey KW, Hedlin H, Rumsfeld JS, Garcia A, Ferris T, Balasubramanian V, Russo AM, Rajmane A, Cheung L, et al. Large-Scale Assessment of a Smartwatch to Identify Atrial Fibrillation. The New England Journal of Medicine. 2019;381:1909-1917
- Rennie KL, Hennings SJ, Mitchell J, Wareham NJ. Estimating energy expenditure by heart-rate monitoring without individual calibration. Medicine and Science in Sports and Exercise. 2001;33:939-45
- Schrack JA, Zipunnikov V, Goldsmith J, Bandeen-Roche K, Crainiceanu CM, Ferrucci L. Estimating energy expenditure from heart rate in older adults: a case for calibration. PLOS ONE. 2013;9:e93520
- Simons-Morton BG, O'Hara NM, Parcel GS, Huang IW, Baranowski T, Wilson B. Children's frequency of participation in moderate to vigorous physical activities. Research Quarterly for Exercise and Sport. 1990;61:307-14
- Sirard JR, Pate RR. Physical activity assessment in children and adolescents. Sports Medicine (Auckland, N.Z.). 2001;31:439-54
- Spurr GB, Prentice AM, Murgatroyd PR, Goldberg GR, Reina JC, Christman NT. Energy expenditure from minute-by-minute heart-rate recording: comparison with indirect calorimetry. The American Journal of Clinical Nutrition. 1988;48:552-9
- Stahl SE, An HS, Dinkel DM, Noble JM, Lee JM. How accurate are the wrist-based heart rate monitors during walking and running activities? Are they accurate enough? BMJ Open Sport & Exercise Medicine. 2016;2:e000106
- Stegle O, Fallert SV, MacKay DJ, Brage S. Gaussian process robust regression for noisy heart rate data. IEEE Transactions on Bio-medical Engineering. 2008;55:2143-51
- Strath SJ, Swartz AM, Bassett DR, O'Brien WL, King GA, Ainsworth BE. Evaluation of heart rate as a method for assessing moderate intensity physical activity. Medicine and Science in Sports and Exercise. 2000;32:S465-70
- Terbizan DJ, Dolezal BA, Albano C. Validity of Seven Commercially Available Heart Rate Monitors. Measurement in Physical Education and Exercise Science. 2002;6(4):243-7.
- Trost SG. Objective measurement of physical activity in youth: current issues, future directions. Exercise and Sport Sciences Reviews. 2001;29:32-6
- Trost SG. State of the art reviews: measurement of physical activity in children and adolescents. American Journal of Lifestyle Medicine. 2007;1(4):299-314
- Wareham NJ, Hennings SJ, Prentice AM, Day NE, Feasibility of heart-rate monitoring to estimate total level and pattern of energy expenditure in a population-based epidemiological study: the Ely Young Cohort Feasibility Study 1994-5. The British Journal of Nutrition. 1998;78:889-900
